Dental Implants - Solutions for missing teeth, even for the most challenging situations
Dental Implant Treatments – UK leaders since 1993
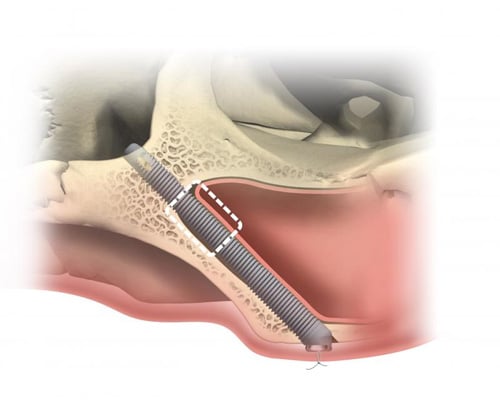
Dr Andrew Dawood has been leading the way with dental implants for over 30 years. Dental Implants offer a reliable solution for replacing missing or failing teeth that feel as natural as your own teeth. Andrew was one of the first to use digital technology, such as 3D Printing and 3D Imaging, to plan and invent new, less invasive techniques. These new methods streamlined the implant process, which greatly improved the success rate for his patients.
Andrew works along with Dr Fiona MacKillop and also collaborates with a team of surgeons on maxillofacial trauma and oncology cases, as well as lecturing internationally. As one of the UK’s leading dental implant surgeons, he is committed to partnering with fellow dental practitioners on more complex implant treatments. He also provides advanced training to his referring dentists to help them and their patients who have missing teeth.
dental implants –everyone is different
Take our questionnaire now for your personalised implant solution.
Before visiting us for a Dental Implant consultation, you can complete our questionnaire which will quickly provide you with an individual report on your specific situation and outline how we can help you with dental implants. You can then arrange an appointment for more detailed information on how to regain your dental function, confidence and your smile.
You will automatically receive your report in an email, and one of our experienced Treatment Coordinators will contact you to discuss your report and help you arrange an appointment.
Exceptional Dental Implant Treatments in London
Replace your missing teeth, improve your smile
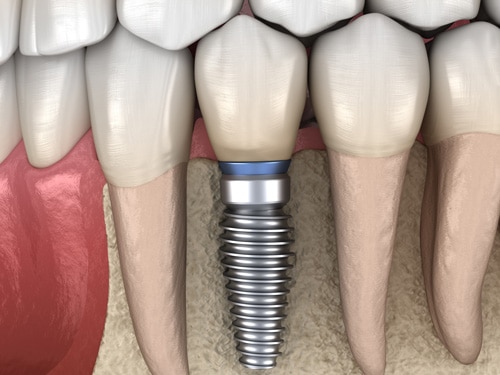
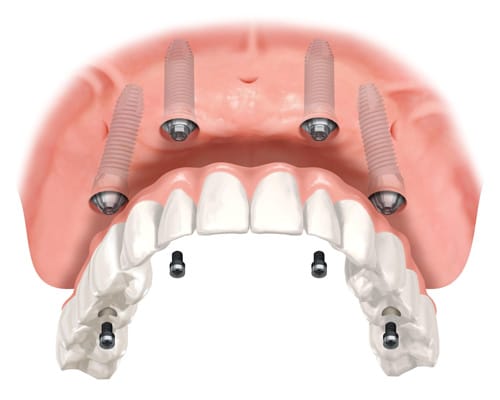
Dental Implants have become the best solution for replacing missing teeth. Whether you are missing a single tooth, or all of your teeth, dental implants are the gold standard. An implant provides a solid, long-lasting, and comfortable solution that looks and feels just like your own natural teeth. An implant supported crown, bridge or denture does more than simply restore your smile, it gives support to your mouth and lips, and this can often lead to a more youthful appearance.
The team have worked for over 30 years to refine every detail of your visit and the dental implant process in order to make it a frictionless experience. In addition to our luxurious dental surgeries, we have a dental imaging suite, and a surgical theatre at the practice, so all of your appointments are in one place. You will have a dedicated treatment coordinator who will guide you through your dental implant journey, and will be available to discuss any questions you may have. You can have peace of mind knowing that your treatment is with a long established practice in the UK, and most importantly our prices include all components.
Our Dental Implant Process and Treatments

I was very scared of the whole process, but it went so smoothly.
At no time did I experience any pain nor discomfort.
The surgeries went so smoothly that I didn't even have to take painkillers the days after any of the surgeries.
The team was thoughtful, attentive, respectful and considerate. I felt very taken care of. Genuinely good people, who happen to be fantastic at their job.
I'm so glad that I went with this amazing team as I was worried having to get implants. But thankfully due to the great work of Dr Dawood and his incredible dental nurse Hannah I never had any problems, any discomfort, any worry that something could go wrong.
I can highly recommend Dawood and Tanner. They are absolutely fantastic.